Some features that we consider abnormal on adult ECGs are completely normal on a child’s ECG. And those features vary by the age of the child.
In the fetus, circulation through the lungs is mostly bypassed, thanks to the patent ductus arteriosus. This means that there is right ventricular dominance, and the right ventricle is larger and thicker than the left ventricle. After birth, the PDA closes and the left ventricle gradually becomes dominant.
Neonates
The newborn’s ECG is similar to the ECG of an adult with right ventricular hypertrophy.
- Axis is rightward. That is, Lead III will have the tallest upright QRS and Leads I and aVL may be negative, short or biphasic, with the axis usually greater than 75 degrees.
- Dominant R wave in Leads V1 - V3. This is because of the relative large size of the right ventricle. There may be an rSR’ pattern, with narrow QRS, in V1. This is called incomplete right bundle branch block. Right bundle branch block has an rSR’ pattern with a wide QRS complex.
- Q waves. Are normal in inferior and left precordial leads - II, III, aVF, V5 and V6.
- Heart rate. The neonate’s heartrate is normally much faster than in adults, peaking around 3 to 8 weeks of age. The usual resting heart rate of the neonate is between 90-190 bpm, though normal ranges vary greatly among references, rising with activity such as crying.
- Cardiac output. Because of a smaller stroke volume, the neonate’s cardiac output is maintained by a faster rate. SV X HR = CO.
- Shorter intervals. The PR interval and QRS duration tend to be shorter, due to the smaller heart size. The QRS may be as short as 30 ms, making the QRS complex very narrow. The PR interval may be as short as 80 ms, and is shorter with faster rates.
- T wave inversion. The juvenile T wave pattern is T wave inversion in V1-V3 that usually occurs during the first week of life and continues until just before adolescence. However, this pattern of T wave inversion may persist until early adulthood.
- Sinus arrhythmia. There is usually marked sinus arrhythmia, with the rate fluctuating with breathing.
Infancy and early childhood
The ECG begins to become more reflective of left ventricular dominance as the child ages from infancy to early childhood.
- Axis moves leftward. The frontal plane axis begins becoming more leftward at 65-70 degrees.
- R wave changes. The R waves in V1-V3 become more normal and shorter than the S waves.
- Q wave amplitude, Q waves in inferior and left precordial leads peak in amplitude at about .6 - .8 mv around 3-5 years.
- Heart rate. The child’s heart rate gradually decreases with age:
- 2 years: 85 – 125 bpm
- 4 years: 75 – 115 bpm
- 6 years: 60 – 100 bpm
- T wave, sinus arrhythmia. Juvenile T wave pattern and sinus arrhythmia persist.
Late childhood and adolescent
As the child ages and enters adolescence the ECG is more like the adult ECG. Some juvenile patterns may persist.
- Axis. Usually normal or slightly to the right (vertical).
- T wave inversions. Juvenile T wave inversions in V1-V3 may persist into early adulthood. Leads which may normally have isolated T wave inversions are Leads III, aVL, aVF, and V1, similar to adults.
- Sinus arrhythmia. Remains common into adolescence.
- Benign early depolarization pattern. Believed to be a normal variant, in young, healthy patients (< 50 years old) is common.
- ST elevation. Widespread modest ST elevation without reciprocal ST depression, especially V2 through V5.
- J point. There is notching or slurring at the J point.
- ST changes. The ST changes are relatively stable, not changing like those due to myocardial infarction.
Pediatric dysrhythmias
These are the most common pediatric dysrhythmias.
Sinus arrhythmia:
- Very common in children.
- Watch for variations with respiratory rate.
- Sinus pauses are frequent in infants, usually less than two seconds and benign.
- Decrease with age.
Sinus bradycardia:
- Common during sleep and in athletic adolescents.
- May slow to a junctional escape rhythm at times.
Sinus tachycardia:
- Common response to fever, dehydration, pain or activity.
Paroxysmal supraventricular tachycardias (PSVT):
- Common dysrhythmias in children, especially in infancy.
- Difficult to differentiate PSVT from ST.
- Look for extremely fast heart rates, abrupt onset and offset, and extremely regular rhythms to recognize PSVT.
- PSVT in infants causes fussiness, irritability, poor feeding and sometimes lethargy.
- PSVT in older children can cause palpitations, dizziness, shortness of breath or chest pain.
Types of PSVT common in children:
- PSVT due to accessory AV pathways, such as Wolff-Parkinson-White syndrome, are more common in infants.
- PSVT with AV nodal reentry pathways are more common in older children.
- While V tach is possible, wide-complex tachycardia in children is most often due to SVT with aberrancy.
AV block:
- AVB is possible, especially in children with anatomic heart defects.
- Because infants’ PR intervals are normally short, a normal PRI may represent a first-degree AVB.
- Second-degree AVB, Type I (Wenckebach) occurs in about 10 percent of normal children and is benign.
PVCs:
- PVCs are common in ambulatory ECGs of children, but rare in resting ECGs.
- Supraventricular ectopics are common and benign in kids.
Bundle branch block:
- Right bundle branch block more common than left bundle branch block.
- Bundle branch block can be associated with congenital malformations or be benign.
- LBBB is rare and you should check for Wolff-Parkinson-White syndrome in wide-complex, supraventricular rhythms, as it is more likely.
Congenital malformations:
Congenital heart malformations occur in eight out of every 1,000 live births. They are often discovered during prenatal exams.
- Congenital malformations can cause conduction abnormalities, chamber enlargements and rhythm disturbances.
- Babies may present with irritability, tachypnea, poor feeding, failure to thrive and congestive heart failure.
Other pediatric cardiac diseases
Many pediatric cardiac diseases can lead to ECG abnormalities, including:
- Myocarditis and cardiomyopathy can cause ECG signs of chamber enlargement, ST changes and QRS morphology changes.
- Kawasaki Disease can cause M.I. signs due to coronary artery aneurysm.
6 12-lead ECG indications
Obtain a 12-lead ECG on any pediatric patient with one or more of these signs or symptoms.
1. Known cardiac history or familial history of sudden cardiac death
2. Cyanosis
3. Loss of consciousness or seizures
4. Drug ingestion or other poisoning
5. Dysrhythmia
6. Chest pain on exertion
Pediatric ECG lead placement
Because the right ventricle is dominant in infants and toddlers, an additional V4 right should be done. You can do a second ECG or just use the V3 wire and label it as “V4R,” skipping V3. The rest of the precordial leads can be placed using the same bony landmarks as for adults.
Limb electrodes should be placed on the limbs, near the shoulders and hips, for less muscle artifact. You can decrease movement artifact in babies if you allow a familiar caregiver to hold them.
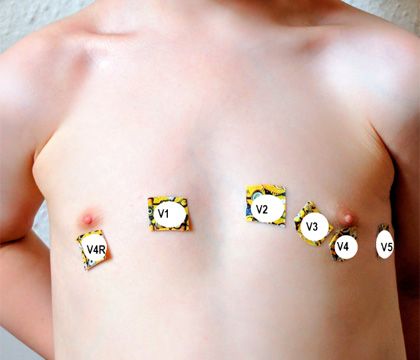
(Photo courtesy of Brooks Walsh)
Bottom line
As with adult ECGs, the best way to determine what findings are abnormal is to be familiar with what normal looks like.
Learn more
Learn more about pediatric ECG acquisition and interpretation from these articles.
















