By David Neubert, MD
What happened: You respond to a house for a “difficulty breathing” patient and find a teenaged male that appears pale and is tachypneic and diaphoretic. He reports that the shortness of breath came on very suddenly. He was diagnosed with strep throat yesterday and has been taking Amoxicillin. He also has been using a throat numbing pain spray “often” because it hurts to swallow.
He is tachypenic, but has a normal work of breathing. His lung sounds are clear, you don’t see retractions, or hear stridor. His tonsils are enlarged and have white patches, but he is swallowing normally.
His vital signs are:
- HR 140
- RR 32
- SpO2 84% while on a non-rebreather
- BP 140/100
- Temp 99 F (37.2 C)
When you start an IV line and draw blood you see the abnormally dark blood in the image.
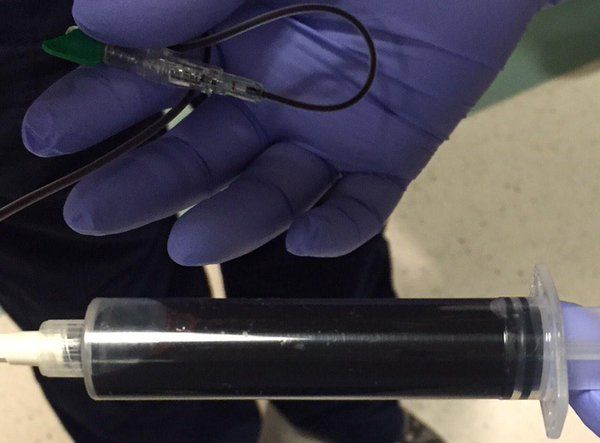
(Photo courtesy Twitter @myERnurselife)
Discussion questions: Teenager with respiratory distress
Discuss these important questions about the patient’s signs and symptoms, as well as the dark-colored blood you withdrew, with your partner, company or squad.
1. What are the most common reasons for a teenager to be dyspneic?
2. What common physical exam findings can be used to help form a differential diagnosis?
3. What could cause blood to be such a dark brown chocolatey color?
4. What further questions would you ask of the patient and family?
5. What additional information would help you solve the mystery in this case?
6. What are your next steps in treatment and care for this patient?
Case discussion
Hemoglobin is the oxygen carrying molecule within the red blood cells. It is iron-based and typically the iron exists in the reduced Fe2+ form. This is the state that effectively binds oxygen, and allows it to be carried through the bloodstream and be delivered to the issues.
A small percentage, typically less than 1 percent, of hemoglobin exits in the oxidized form Fe3+. When hemoglobin is oxidized it loses an electron to another molecule. This form of hemoglobin, called methemoglobin, is dark brown and does not carry oxygen. This causes a functional anemia.
In certain situations, the levels of methemoglobin in the blood become very high, and this causes acute distress from hypoxemia, as the blood loses its ability to carry oxygen. The most common causes of this are toxin or drug exposures. There are some people that have congenital methemoglobinemia due to certain enzyme deficiencies.
The most common reasons for acquired methemoglobinemia are the following (adapted from the EMedicine):
- Organic and inorganic nitrate exposure from cardiac nitrates (nitroglycerin), blood pressure control medications (nitroprusside), anesthetics (nitric oxide), and even foods (i.e. hot dogs and cured meats).
- Chlorate exposures from matches, explosives and fungicides.
- Topical and injected local anesthetics such as link benzocaine, lidocaine, prilocaine, phenazopyridine, silver sulfadiazine (used in burn care).
- Other exposures routes include smelling salts, weight loss agents, PCP, cocaine, chemotherapy agents, analgesics and antipyretics, herbicides and insecticides, certain antibiotics (sulfa drugs), naphthalene (moth balls) and nitroethane (nail polish remover).
Based on the patient’s symptoms, which of these causes seems most likely?
Remember these signs of methemoglobinemia:
- Dyspnea
- Cyanosis
- Blood and skin discoloration
- Arrhythmias
Coma, seizures and unconsciousness are also possible as the ability to deliver oxygen decreases.
Prehospital treatment for a patient with methemoglobinemia involves improving oxygen carrying capacity of the blood and reducing the hemoglobin back to the Fe2+ state so that it can carry oxygen again. To do this administer high-flow oxygen and intravenous fluids. Consider sodium bicarbonate as a temporizing measure if the patient is acidotic.
The first line treatment in the emergency department is Methylene blue, which is a medication that acts as an electron donor and helps to reduce the hemoglobin. Blood transfusion or hyperbaric oxygen are additional treatment options.

Learn more about methemoglobinemia from EMedicine, Medline plus and UpToDate.
The blood of a patient with methemoglobinemia. Lesson: Don’t try to kill yourself by drinking acrylic nail hardener. pic.twitter.com/Oy52XmOho5
— myERnurselife (@myERnurselife) January 13, 2015
About the author
David Neubert, MD is an emergency physician that is board certified in Emergency Medical Services. He is medical director of Tac-Med, LLC, which provides on-line and hands on training in dynamic threat medical response for emergency responders. He can be contacted at DNeubert@tac-med.org.











