Editor’s note: We asked columnist Tom Bouthillet to pick a winner to this month’s challenge and he wrote: For this case I’m selecting Michael Schadone. He picked up on the limb lead reversal and correctly considered pericarditis in his differential diagnosis. Congratulations, Michael! Thanks for participating.
This is the solution to the ECG Challenge: A horse or a zebra? You may wish to go back and review the history and clinical presentation.
Let’s take another look at the initial 12-lead ECG.
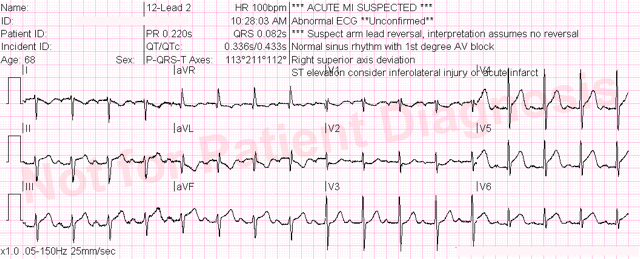
Any time I have a patient with: 1) a chief complaint of chest discomfort, 2) who receives a 12-lead ECG that shows excellent data quality, and 3) the ***ACUTE MI SUSPECTED*** message appears at the top, it gets my attention.
At first glance this appears to be an obvious case of acute inferolateral STEMI. ST-elevation is present in the inferior leads and low lateral leads. Importantly, there is a downsloping ST-segment in lead aVL (which we all know by now strongly supports the diagnosis of acute inferior STEMI) and we also see ST-depression in lead V2.
Based on these findings, the treating paramedic called a “Code STEMI” from the field and treated the patient with oxygen, aspirin and nitroglycerin.
While en route to the hospital the paramedic noticed that the arm leads were reversed. This problem was corrected and the following 12-lead ECG was obtained.
This is no longer a slam-dunk ECG diagnosis. The ST-elevation in the inferior leads is now maximal in lead II over lead III. In addition, the ST-segments are no longer downsloping in leads I and aVL. ST-elevation is still present in leads V5 and V6, but we now must move up pericarditis on our list of differentials. I’m not saying this ECG can easily be blown off! There is still a dip in the ST-segment in lead V2, which I don’t like and can be construed as a reciprocal change.
The ED physician apparently agreed, and the patient was sent emergently to the cardiac cath lab where the patient was found to have clean coronaries. The diagnosis was pericarditis.
Pericarditis is actually a fairly uncommon STEMI mimic, and some ECG experts like our good friend Stephen Smith, M.D. from Dr. Smith’s ECG Blog argue that many cases thought to be pericarditis are actually missed STEMIs.
Sometimes the best thing to do is send a patient to the cath lab. An ECG like this with a suggestive clinical presentation should be considered an acceptable cath lab activation, even when it turns out not to be STEMI.
This case is also a lesson that inadvertently crossing limb leads can have real consequences for patient care.













