Updated July 18, 2017
I am a victim. Yup, it’s true.
A victim who has been “intubated” on numerous occasions, has had a rescue airway “inserted,” been bagged, been fully c-spined – too many times to remember – and turned upside down on the board to prove that I really was securely strapped.
I have been a severely injured, intubated trauma patient in a public education video on traffic safety when ambulances are using lights and sirens. I have had numerous IVs started and have had CPAP administered in several instances.
Yes, I am a victim. If I lived in California, I feel confident I would have long ago discovered and enrolled in a support group for victimized EMS medical directors.
But I don’t live in California; I live in Colorado Springs, Colorado, the home of the U.S. Air Force Academy, many retired military and more evangelical religious organizations than Paris Hilton has court appearances.
As a result, while I don’t know for sure, I think support groups might be illegal in our town. So maybe that’s why I have yet to find a support group for people like me in our area. Woe is me.
Recently, I was the victim again. Our agency decided to take a look at a new alternative to the mask (as in “bag–valve–mask”).
The FDA approved device is called the NuMask IntraOral Mask. Invented by three California emergency physicians, it fits into the patient’s mouth kind of like the hose from a SCUBA tank regulator. It can be used to ventilate patients with or without a gag reflex.
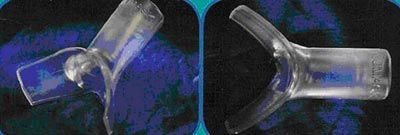 |
| The NuMask with oral sealing flanges and central stem to connect with the ventilating bag |
A paramedic from a neighboring agency first saw it and told me about it. I contacted one of the inventors, David Isagholian, M.D., and asked if I could have one or two samples for an upcoming airway lecture I was giving. He provided the sample and we have stayed in touch since.
While we have not yet used the NuMask in actual clinical situations, we are beginning a trial utilizing a limited number of ambulances staffed by our Field Training Officers after introduction and coordination with our local fire department EMS partners.
Last week, Isagholian happened to be in Colorado and visited us at our agency headquarters. That began my most recent odyssey into victimhood. We needed a sample patient to demonstrate the NuMask and, via the usual process of elimination, I was selected. What follows is a pictorial depiction of how to insert and use the NuMask.
All I can say is despite what your eyes may tell you, I was not deceased during the session (though that table I’m lying on was pretty close to a slab at the morgue). Anyway, without further ado, here we go.
 |  | |
| 1. The NuMask being inserted into the right side of my mouth. | 2. The NuMask inserted into the right side of my mouth. | |
 |  | |
| 3. The NuMask being inserted into the left side of my mouth. | 4. The completed insertion. | |
 |  | |
| 5. Isagholian hooking up the bag-valve-mask. | 6. The BVM hooked up to the NuMask. | |
 |  | |
| 7. Various hand positions to seal the NuMask. | 8. Pinching the nose to facilitate the seal. | |
 |  | |
| 9. Attaching a prototype strap to occlude the nose. | 10. Bagging via the NuMask with the prototype strap in place. (learn how to improve your bag-valve mask technique) |
|
Depiction of how the NuMask fits in mouth with hand positions to seal it against the face |
After viewing the pictures, here a few thoughts – besides just how God-awful I look.
- There are a few different hand positions that can be used to facilitate the seal of the NuMask. After we complete our trial over the next several months, I will outline the hand positions in more detail in a follow up article.
- The manufacturer is working on a prototype strap that will be somewhat similar to the one pictured. The idea is that the strap will seal the nose and mouth, ideally permitting only “one-hand” use by the rescuer to just squeeze the bag. No contact will be necessary with the NuMask and the patient’s face when using the strap.
- With the use of a strap, the NuMask may be used with any commercially available CPAP machine. The CPAP circuit can be simply connected to the stem of the NuMask and the process started without the use of a standard mask.
- The NuMask may be used either with a supplied oral airway or no airway adjunct. If the patient has a gag reflex and/or the patient is awake, no oral airway should, of course, be needed. However, the recommendation is that, even if the patient does not have a gag, the NuMask be used initially without the oral airway. If it appears an oral airway is necessary, the supplied one is the only one that should be used. It is a softer airway with a smaller flange at the lips so that the airway fits well underneath the oral seating surface of the NuMask.
- The NuMask can be used with an endotracheal tube-type capnography probe. We are anxious to review the capnography data at AMR Colorado Springs. But the stem of the NuMask is 22 mm and the standard endotracheal tube tip is 15 mm. So in order to get the capnography data using the NuMask, we will have to locate an adapter that reduces the size of the stem to 15 mm.
Once we have gathered data over the next few months regarding ease of use for the crews, effectiveness of ventilations, pulse oximetry, capnography, patient comments, pertinent comments from receiving emergency department staff, as well as any patient outcome reports, I will pass the information on to you in a subsequent column.
Stay healthy and be safe.
Author’s note: This column is the first in a quarterly series on EMS1.com. I will be chronicling some of the newer products, skills and drugs we have considered at my base agency, AMR, Colorado Springs, Colo. Due to contractual obligations with the local and regional area, our agency runs a lot of calls in varied environments. As such, we have trialed a variety of equipment in past years and continue to do so. These are not peer-reviewed trials or scientific studies. Nevertheless, over the years at our agency, we have often gathered data that has helped us determine whether or not the equipment might be suitable for our mission. This information may be of use to your agency in the event you haven’t had an opportunity to analyze this equipment yet, or may not be aware that it exists in the market. I wholeheartedly encourage readers or vendors with knowledge of products that might be interesting for us to cover in Out of the Box to email me at drdr0682@aol.com. I encourage input from all sectors of the EMS arena. Please let me make perfectly clear that I receive no payment or consideration of any kind from any vendor or manufacturer related to any product discussed in this column.














